 A new study led by Dr. Barry Maron at the Minneapolis Heart Institute Foundation (MHIF) and Dr. Martin Maron at Tufts Medical Center in Boston revealed a paradigm shift in the clinical progression of hypertrophic cardiomyopathy (HCM). The study was recently published in the journal Trends in Cardiovascular Medicine and is entitled “The 20 advances that have defined contemporary hypertrophic cardiomyopathy.”
A new study led by Dr. Barry Maron at the Minneapolis Heart Institute Foundation (MHIF) and Dr. Martin Maron at Tufts Medical Center in Boston revealed a paradigm shift in the clinical progression of hypertrophic cardiomyopathy (HCM). The study was recently published in the journal Trends in Cardiovascular Medicine and is entitled “The 20 advances that have defined contemporary hypertrophic cardiomyopathy.”
HCM corresponds to a genetic heart disease in which the myocardium (the heart muscle) becomes abnormally thick (hypertrophied). People with HCM can live normal, healthy lives, although some may suffer cardiac problems that can have an impact on their quality of life. HCM can be fatal, and in some particular cases, it can result in a dangerously fast heart rhythm that can cause sudden cardiac death (SCD), a condition that has been reported in healthy young athletes.
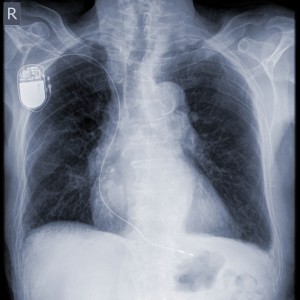
Technology and research advances in the past 10-15 years allowed the improvement of treatment options for adults with HCM. Implantable defibrillators (ICDs) were originally conceived to prevent SCD in coronary artery disease patients, being now often recommended in individuals with HCM at high risk for sudden death. ICDs deliver a shock to the heart when they detect a dangerously fast heartbeat, restoring normal heart rhythm.
The team wanted to determine the impact of the advances in care, especially ICDs, on the clinical course of HCM from an odd and exotic disease to a contemporary and treatable disease. As such, researchers analyzed the long-term outcomes, namely death rates and causes of death, in 1,000 adult patients with HCM between 1992 and 2011.
Researchers found that patients with HCM have benefitted from ICDs and other modern treatments that have led to a reduction in mortality rates and a normal life expectancy. In fact, the mortality rates among HCM patients were found to be similar to the death rates among the general population. “Today’s treatment interventions, including ICDs for SCD prevention (an initiative started here at MHIF), have dramatically changed the outlook for these patients,” said Dr. Barry Maron in a news release. “They are living longer and deaths directly associated with the disease are much less common, especially those caused by SCD.”
The researchers found that in the follow-up period analyzed, 4% of the patients had succumbed to an HCM-associated death, while 6% had experienced and survived a life-threatening episode in the majority attributed to an ICD. Remarkably, of the 17 reported HCM sudden deaths, 6 had occurred in patients who refused ICD therapy and 11 occurred in patients without risk factors that justified ICD therapy or in patients who were attended in the 1990s before ICDs were generally employed for HCM.
This study “changes our perceptions of HCM from a grim, unrelenting, and largely untreatable condition to a contemporary disease with effective treatment options and a low rate of death,” concluded Dr. Barry Maron.


