Congenital heart experts at Spectrum Health Helen DeVos Children’s Hospital in Grand Rapids, Michigan, have successfully integrated two common imaging techniques — echocardiography and CT — to produce a three-dimensional anatomic model of aCongenital heart experts sat Spectrum Health Helen DeVos Children’s Hospital in Grand Rapids, Michigan, have successfully integrated two common imaging techniques — echocardiography and CT — to produce a three-dimensional anatomic model of a patient’s heart.
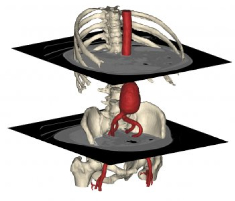
In recent years, 3D anatomical reconstructions from medical images have become an established tool for diagnostics, educational purposes and intervention planning in fields of orthopedics, cranio-maxillo-facial surgery and others, and use of printed, physical models of these 3D anatomical reconstructions is also being increasingly adopted in cardiovascular medicine over the past few years — part of an emerging, experimental field of medical technology dedicated to enhanced visualization of individual cardiac structures and characteristics.
However, this is the first time integration of computed tomography (CT) and three-dimensional transesophageal echocardiography (3DTEE) has successfully been employed to print a hybrid 3D model of a patient’s heart, and a proof-of-concept study authored by Spectrum Health experts opens the way for these techniques to be used in combination with a third technology — magnetic resonance imaging (MRI).
“Hybrid 3D printing integrates the best aspects of two or more imaging modalities, which can potentially enhance diagnosis, as well as interventional and surgical planning,” says Jordan Gosnell, Helen DeVos Children’s Hospital cardiac sonographer, and the study’s lead author. “Previous methods of 3D printing utilize only one imaging modality, which may not be as accurate as merging two or more datasets.”
The team used specialized software capable of registering images from the two imaging modalities to selectively integrate datasets and produce an accurate anatomic model of the heart. The result creates more detailed and anatomically accurate 3D renderings and printed models, which may enable physicians to better diagnose and treat heart disease.
Computed tomography (CT) and magnetic resonance imaging (MRI) are established imaging tools for producing 3D printable models. Three-dimensional transesophageal echocardiography (3DTEE) recently was reported by Joseph Vettukattil, MD, and colleagues at Helen DeVos Children’s Hospital to be a feasible imaging technique to generate 3D printing in congenital heart disease. Dr. Vettukattil is co-director of the Helen DeVos Children’s Hospital Congenital Heart Center, division chief, pediatric cardiology, and senior author of the study.
According to Dr. Vettukattil and his research team, each of these imaging tools brings particular strengths, which can improve and enhance 3D printing. While CT enhances visualization of the outside anatomy of the heart, MRI is superior to other imaging techniques for measuring the interior of the heart, including the right and left ventricles or main chambers of the heart, as well as the heart’s muscular tissue, and 3DTEE provides the best visualization of valve anatomy.
“This is a huge leap for individualized medicine in cardiology and congenital heart disease,” Dr. Vettukattil observes. “The technology could be beneficial to cardiologists and surgeons. The model will promote better diagnostic capability and improved interventional and surgical planning, which will help determine whether a condition can be treated via transcatheter route or if it requires surgery.”
Dr. Vettukattil is known internationally for his work and research with three- and four-dimensional echocardiography. Most notably, he developed the advanced technique of multiplanar reformatting in echocardiography, a method used to slice heart structures in infinite planes through the three dimensions in a virtual environment similar to a cardiac pathologist dissecting the heart to reveal underlying pathology. Dr. Vettukattil devised the concept of integrating two or more imaging modalities for 3D printing, and pioneered multiplanar reformatting’s use in echocardiography to evaluate complex heart defects. The technique is now commonly used collaboratively with other diagnostic technologies, such as CTs.
Dr. Vettukattil presented the findings of the proof-of-concept study, entitled “A new device for diastolic left heart and right heart failure,” on June 25 at the CSI 2015 – Catheter Interventions in Congenital, Structural and Valvular Heart Diseases Congress held June 24-27 in Frankfurt, Germany, to demonstrate the feasibility of printing 3D cardiovascular models derived from multiple imaging modalities.
 The Helen DeVos Children’s Hospital team worked with the Mimics Innovation Suite software from Materialise, a provider of 3D printing software and services based in Belgium, which printed the model using its HeartPrint Flex technology. HeartPrint is Materialise’s service for providing 3D-printed cardiovascular models from medical image data. A white paper on HeartPrint can be found here:
The Helen DeVos Children’s Hospital team worked with the Mimics Innovation Suite software from Materialise, a provider of 3D printing software and services based in Belgium, which printed the model using its HeartPrint Flex technology. HeartPrint is Materialise’s service for providing 3D-printed cardiovascular models from medical image data. A white paper on HeartPrint can be found here:
http://biomedical.materialise.com/white-papers-material-characteristics-heartprint-flex-models-abstract
Dr. Gosnell worked on integration of the imaging modalities in collaboration with Materialise’s US Headquarters in Plymouth, Michigan to produce the final 3D rendering. Mimics is software developed by Materialise for medical image processing and used for the segmentation of 3D medical images (coming from CT, MRI, micro-CT, CBCT, 3D Ultrasound, Confocal Microscopy) and enabling production of highly accurate 3D models of a patient’s anatomy. The Mimics Innovation Suite is a complete set of tools consisting of several modules and other complementary software solutions and services developed for biomedical professionals, that allow clinicians to perform a variety of engineering operations starting from medical imaging data.
The investigators note that further research is required to evaluate the efficacy of hybrid 3D models in decision-making for transcatheter or surgical interventions.
Spectrum Health is a not-for-profit health system, based in West Michigan, offering a full continuum of care through the Spectrum Health Hospital Group, which is comprised of 12 hospitals, including Helen DeVos Children’s Hospital; 180 ambulatory and service sites; 1,300 physicians and advanced practice providers, which include 1,100 members of the Spectrum Health Medical Group; and Priority Health, a health plan with more than 648,000 members.
Spectrum Health sees maintaining a progressive research culture in Grand Rapids as fundamental to its role as the region’s largest medical center, and it continues to grow its own research accomplishments as well as build collaborative relationships within and throughout the local research community.
More than 750 open research studies are approved through Spectrum Health’s Institutional Review Board, and more than 220 national cancer clinical trials through the Grand Rapids Clinical Oncology Program
More information on current research studies can be found at the Spectrum Health Research & Clinical Trials website:
http://www.spectrumhealth.org/research
Spectrum Health is West Michigan’s largest employer, with 22,600 employees. The organization provided $294.6 million in community benefit during its 2014 fiscal year. Spectrum Health is the only health system in Michigan to be named one of the nation’s 15 Top Health Systems by Truven Health Analytics for 2015 — the fourth time the organization has received this recognition.
Sources:
Spectrum Health
Materialise
Image Credits:
Spectrum Health
Materialise


