The cardiothoracic surgery team at Wake Forest University Baptist Medical Center in Winston-Salem, NC performed a clinical trial to evaluate the effectivness of a sternal support device in patients with a high-risk for developing sternal wound dehiscence and/or infection after they are submitted to cardiac surgery.
While few studies have focused on sternal support harnesses, a study from 2000 suggests that patients experience positive benefits from using a sternum support device.
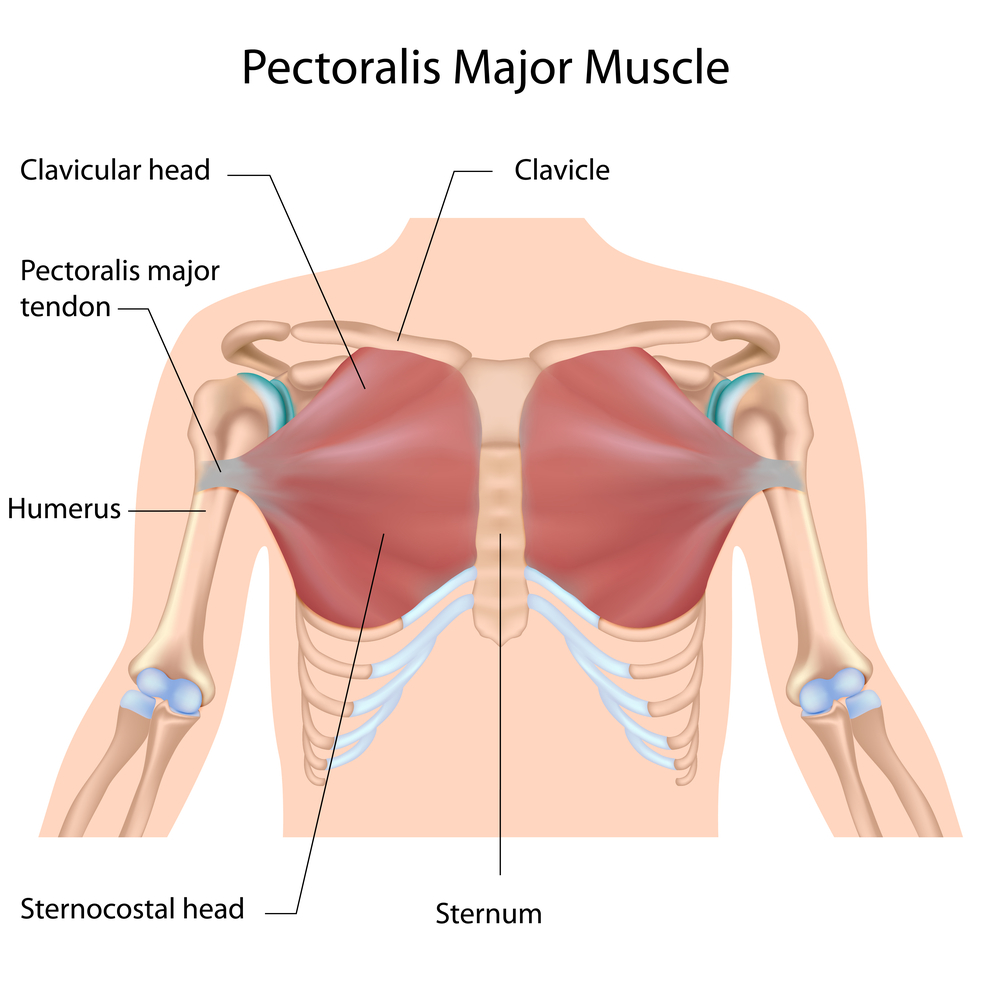
At Wake Forest University Baptist Medical Center, 4% of all readmissions related to cardiac surgery are due to post-surgery complications, particularly infections, mediastinitis (inflammation of the tissues in the mid-chest) and wound dehiscence (wound rupturing along the surgical suture). The team, however, highlights that patient noncompliance with after-surgery guidelines are key in increasing their risk for post-surgery complications. This factor is particularly worrisome in high-risk patients, i.e., those that have diabetes, increased weight (above 250 pounds), large chest and/or pendulous breasts, redo sternotomy or those that used bilateral mammary arteries for coronary bypass grafts.
The current guidelines clearly state that patients need to support the sternum whenever they take a deep-breath or during coughing. Additionally, patients are forbidden to either push or pull objects, and cannot lift objects heavier than 10 pounds.
To evaluate the effect of a sternal support harness in these high-risk patients, the cardiothoracic surgery team placed the device in selected patients immediately after extubation. To increase the device effectiveness, besides patients, family members and nursing staff were also taught how to apply the device into patients. During their hospital stay, patients reported their pain level and device compliance.
In general, patients benefitted with the sternal support device, reporting lower levels of pain, increased compliance with post-surgery guidelines, and enhanced mobility. From the pool of patients evaluated (n=19), only 2 patients were readmitted due to sternal wound infections.
In light of these results, hospital’s Product Evaluation Committee approved the sternal support harness to be introduced in the post-surgery guidelines and a must use for all high-risk patients. This measure is expected to decrease the cost associated with cardiac surgery-related readmissions, since 30 to 40% of all adults that undergo cardiac surgery at Wake Forest are at risk for wound dehiscence.