 The U.S. Food and Drug Administration (FDA) recently approved the first fully absorbable stent for treating coronary artery disease.
The U.S. Food and Drug Administration (FDA) recently approved the first fully absorbable stent for treating coronary artery disease.
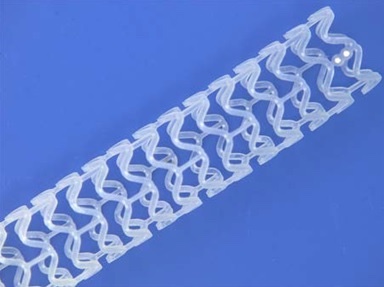
The Absorb GT1 Bioresorbable Vascular Scaffold System (BVS), a device manufactured by Abbott Vascular in Santa Clara, California, gradually releases the drug everolimus to limit growth of scar tissue, and biodegrades to be absorbed by the body in about three years, leaving behind only two platinum marker beads embedded in the arterial walls, which help identify where the stent was originally placed.
Stents are tiny mesh tubes, usually made of wire, that are inserted in a constricted artery using a balloon catheter procedure called percutaneous coronary intervention (PCI) — also known as “angioplasty with stent.” The balloon is inflated when the stent is in position, expanding it to secure it in place holding the artery open and allowing blood to flow more freely.
Stents have traditionally been left in place permanently, but the FDA notes that scar tissue can form within the stent causing the artery to narrow again (restenosis). Drug-eluting stents temporarily release a drug, typically for a few months after stent placement, to combat scar tissue formation.
 Instead of metal wire, the Absorb GT1 stent is made of an absorbable, biodegradable polymer, poly(L-lactide) (PLLA), which is similar to materials used in other types of absorbable medical devices, such as sutures. It is coated with another absorbable polymer called poly(D,L-lactide) (PDLLA) containing the drug everolimus which had previously been approved by the FDA for treating other diseases, including several types of cancers.
Instead of metal wire, the Absorb GT1 stent is made of an absorbable, biodegradable polymer, poly(L-lactide) (PLLA), which is similar to materials used in other types of absorbable medical devices, such as sutures. It is coated with another absorbable polymer called poly(D,L-lactide) (PDLLA) containing the drug everolimus which had previously been approved by the FDA for treating other diseases, including several types of cancers.
The absorbable stent incorporates the two platinum marker beads — one embedded at each end. The delivery system is comparable to the one used in Abbott Vascular’s XIENCE Alpine Coronary Stent System (CSS).
 “The FDA’s approval of the Absorb GT1 BVS offers a new treatment option for individuals who are candidates for angioplasty, but would prefer an absorbable device rather than a permanent metallic coronary stent,” Bram Zuckerman, MD, director of the division of cardiovascular devices at the FDA’s Center for Devices and Radiological Health, said in a press release.
“The FDA’s approval of the Absorb GT1 BVS offers a new treatment option for individuals who are candidates for angioplasty, but would prefer an absorbable device rather than a permanent metallic coronary stent,” Bram Zuckerman, MD, director of the division of cardiovascular devices at the FDA’s Center for Devices and Radiological Health, said in a press release.
The absorption of the device by the body gradually eliminates the presence of foreign material in the artery once the stent is no longer needed. After absorption, there are only four very small platinum markers embedded in the walls of the artery, which help cardiologists identify where the Absorb GT1 BVS was originally placed.
During the Absorb GT1 BVS approval vetting process, the FDA evaluated data from a large randomized clinical trial of 2,008 patients in the U.S. (ABSORB III) that compared the combined rate of major adverse cardiac events between the Absorb GT1 BVS and the XIENCE metallic drug-eluting metal stent.
The study found that after one year, the Absorb GT1 BVS group had a major cardiac adverse event rate of 7.8 percent, clinically comparable to a rate of 6.1 percent observed in the control group. Additionally, after a year, the rates of blood clots forming within the devices were 1.54 percent and 0.74 percent, respectively.
An additional analysis showed that the use of Absorb to treat blockages in small heart arteries was associated with an increased risk of cardiac events (primarily heart attack and blood clot formation within the scaffold) compared to treatment with the XIENCE stent. To address this issue, the FDA’s instructions for use include specific information regarding the importance of vessel sizing to identify arteries for which Absorb implantation is appropriate.
In summary, the FDA concluded that “overall, clinical outcomes in the Absorb group were comparable to XIENCE, and demonstrated that the Absorb GT1 BVS is safe and effective for patients for whom the device is intended.”
Coronary heart disease causes approximately 370,000 deaths in the U.S. each year, according to National Heart, Lung, and Blood Institute metrics. The disease develops when cholesterol-containing deposits build up on the inner walls of coronary arteries, diminishing blood flow to the heart, which can cause chest pain (angina), shortness of breath, fatigue, and other heart disease symptoms.

