A new study called INTERSTROKE revealed that 10 modifiable risk factors account for 90 percent of strokes globally, with hypertension listed as the most important. The relative role of each risk factor depends on the region, suggesting that the strategies for reducing the risk of stroke should be adapted to individual regions.
The findings were published in the journal The Lancet in the study “Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study,” and result from a collaborative effort of researchers at the Population Health Research Institute at McMaster University in Canada, and investigators from 32 other countries.
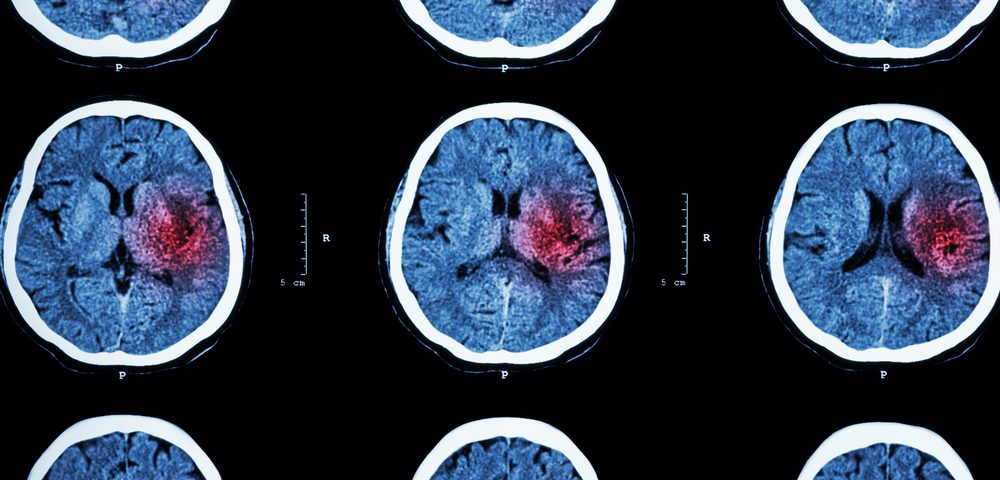
Stroke is one of the leading causes of death worldwide. There are two major types: ischemic stroke, caused by blood clots, and hemorrhagic stroke, which is characterized by brain bleeding.
Preventing stroke is a major concern for public health entities, but there is a need to understand which are the key preventable causes of stroke.
Preliminary results from the INTERSTROKE study allowed researchers to identify 10 risk factors in 6,000 participants from 22 countries. Then, 20,000 more subjects from 32 countries were included to understand whether the main causes of stroke were distinct in diverse populations.
“This study is of an adequate size and scope to explore stroke risk factors in all major regions of the world, within key populations and within stroke subtypes,” said Dr. Martin O’Donnell from the Population Health Research Institute at McMaster University, and the HRB-Clinical Research Facility, NUI Galway, Ireland, in a press release.
“The wider reach confirms the 10 modifiable risk factors associated with 90 percent of stroke cases in all regions, young and older and in men and women. The study confirms that hypertension is the most important modifiable risk factor in all regions, and the key target in reducing the burden of stroke globally,” O’Donnell said.
To understand the contribution of each risk factor, researchers estimated the overall disease burden that could be reduced after eliminating that specific risk factor, in a measure called population attributable risk factor (PAR).
Hypertension had the highest PAR (47.9%), followed by physical activity (35.8%), lipids (26.8%), poor diet (23.2%), obesity (18.6%), smoking (12.4%), heart diseases (9.1%), alcohol intake (5.8%), stress (5.8%), and diabetes (3.9%). Combined, the total PAR for all 10 risk factors was 90.7%, a percentage that was similar across all age groups, regions, and gender.
Although the total PAR remained similar, the role of some risk factors varied by region. Hypertension, for instance, had the highest PAR in Southeast Asia (59.6%) and the lowest in North America, Australia, and western Europe (38.8%).
“INTERSTROKE demonstrates that the majority of stroke is due to common modifiable risk factors,” said Prof. Salim Yusuf, who led the study with O’Donnell. “Our findings will inform the development of global population-level interventions to reduce stroke, and how such programs may be tailored to individual regions, as we did observe some regional differences in the importance of some risk factors by region. This includes better health education, more affordable healthy food, avoidance of tobacco, and more affordable medication for hypertension and dyslipidaemia.”
“Three key messages can be drawn from this study,” wrote Prof. Valery L. Feigin and Dr. Rita Krishnamurthi from the National Institute for Stroke and Applied Neurosciences, Faculty of Health and Environmental Sciences at the University of Technology in Auckland, New Zealand, in a comment to the study.
“First, stroke is a highly preventable disease globally, irrespective of age and sex. Second, the relative importance of modifiable risk factors and their PAR necessitates the development of regional or ethnic-specific primary prevention programs, including priority settings such as focusing on risk factors contributing most to the risk of stroke in a particular region (as determined by PAR).
“Third, additional research on stroke risk factors is needed for countries and ethnic groups not included in INTERSTROKE, as well as definitive cost-effectiveness research on primary stroke prevention in key populations (eg, different age, sex, ethnicity, or region).”