In a collaboration between the MIT and the Boston Children’s Hospital, researchers were able to develop a new system capable of taking magnetic resonance imaging (MRI) scans of the heart and, in a short time, convert the scans into a physical model that surgeons can utilize to prepare surgery. The new system will be presented at the upcoming International Conference on Medical Image Computing and Computer Assisted Intervention.
“Our collaborators are convinced that this will make a difference,” said in a news release Polina Golland, a professor of electrical engineering and computer science at MIT, who led the project. “The phrase I heard is that ‘surgeons see with their hands,’ that the perception is in the touch.”
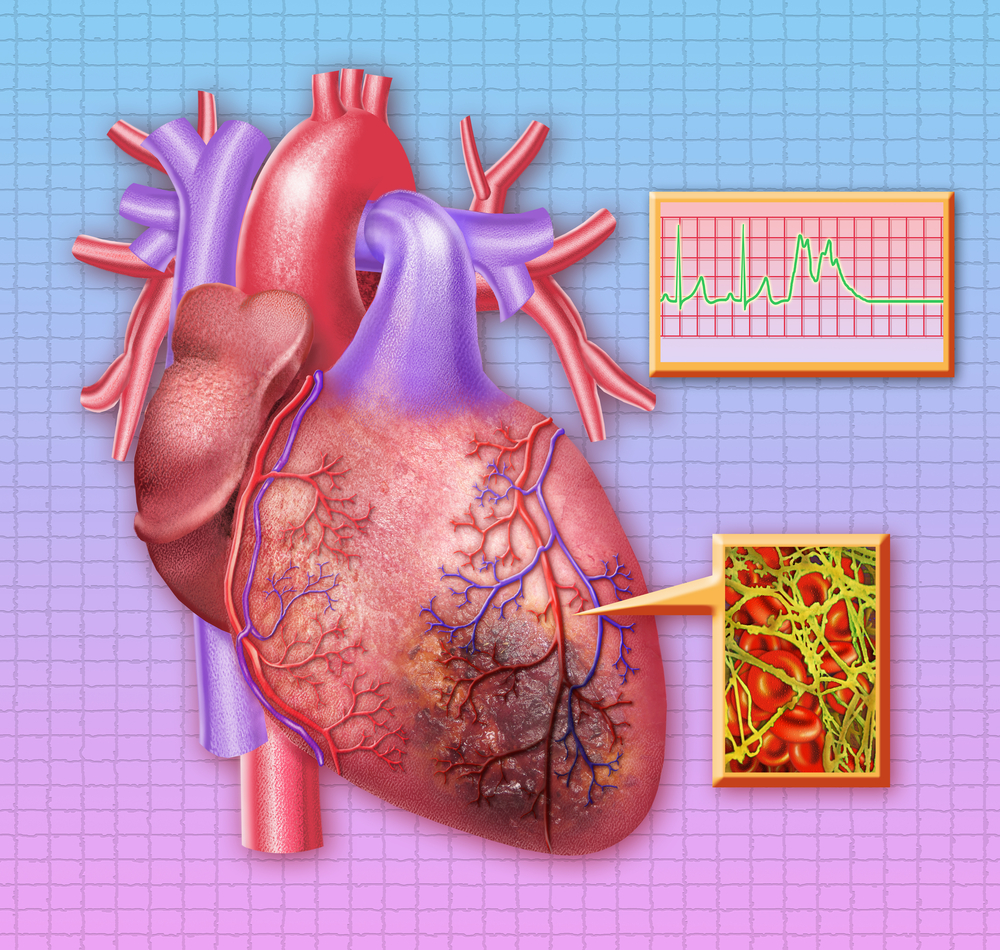
MRI scans involve a series of cross sections of a three-dimensional entity. Each section has light and dark regions and the boundaries of the regions indicate edges of anatomical structures. Image segmentation is one of the main problems of computer vision, since it is hard to delimit the boundaries of different objects in an image. Furthermore, image-segmentation algorithms aren’t consistent to produce precise models that could be used by surgeons to plan clinical procedures.
To increase the precision of an image-segmentation algorithm there is the need to enhance the model size. In the case of human hearts, these have chambers and blood vessels that are typically size-consistent. The heart anatomical consistency could provide to a segmentation algorithm a manner to avoid questionable conclusions about object boundaries. However, many patients undergoing cardiac surgery have an irregular anatomy of their hearts.
Researchers have produced in past printable heart models by indicating the boundaries manually in MRI scans. However, this can be a lengthy process, taking up to 10 hours. “They want to bring the kids in for scanning and spend probably a day or two doing planning of how exactly they’re going to operate,” Dr. Golland said. “If it takes another day just to process the images, it becomes unwieldy.”
The research team’s solution to address this issue was to ask a human specialist to ascertain boundaries in the cross sections and allow algorithms to conclude the process. The most interesting results arose when the researchers asked the specialist to segment a small patch, about one-ninth of the total region. The segmentation of 14 patches and allowing the algorithm to infer the rest, yielded 90% consensus with the specialist segmentation of the whole 200 cross sections. Human segmentation of just 3 patches yielded 80% consensus.
“I think that if somebody told me that I could segment the whole heart from eight slices out of 200, I would not have believed them,” Dr. Golland said. “It was a surprise to us.”
Human segmentation of sample patches and the algorithmic generation of a digital, 3-D model of the heart takes roughly one hour. The process of the 3-D-printing takes approximately two more hours.
During this fall, seven cardiac surgeons from the Boston Children’s Hospital will conduct a new study that will assess the usefulness of these heart models. The study will involve MRI scans from 10 patients, and all the surgeons will have access to the patients’ information, including raw MRI scans and either a computerized 3-D model or a physical model. The model will be based on algorithmic segmentations or in human segmentations.
With this information, heart surgeons will develop their surgery plans, which will then be compared with clinical information about the interventions that each patient underwent. The aim of the study is to assess if 3-D-printed physical models can improve surgical clinical outcomes.
“Absolutely, a 3-D model would indeed help,” said Sitaram Emani, a cardiac surgeon at Boston Children’s Hospital who was not involved in the research. “We have used this type of model in a few patients, and in fact performed ‘virtual surgery’ on the heart to simulate real conditions. Doing this really helped with the real surgery in terms of reducing the amount of time spent examining the heart and performing the repair.”
“I think having this will also reduce the incidence of residual lesions — imperfections in repair — by allowing us to simulate and plan the size and shape of patches to be used,” concluded Emani. “Ultimately, 3D-printed patches based upon the model will allow us to tailor prosthesis to patient. (…) Finally, having this immensely simplifies discussions with families, who find the anatomy confusing, (…) This gives them a better visual, and many patients and families have commented on how this empowers them to understand their condition better.”